|
For more information call
The Wellington Hospital: 020 7483 5589
Fortius Clinic: 0845 853 1000 The Yorkshire Clinic: 01274 621600 |
Hip Conditions ~ Miscellaneous
Snapping hip syndrome (Coxa saltans)
Snapping hip syndrome is a condition characterised by a snapping sensation when the hip is moved. The anatomical structures that are usually causing the audible clunk are the Iliotibial band and the psoas tendon. Both of these types are extra-articular, which means that these structures are lying outside the joint capsule.
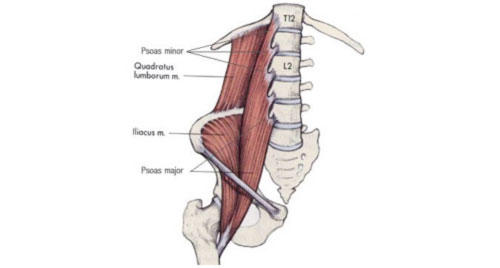
(Figure demonstrating the anterior muscles of the thigh)
(Figure demonstrating where the psoas tendon runs of the rim of the acetabulum.)
Snapping Iliopsoas tendon
The medial type of snapping hip occurs when the Ilio psoas tendon moves from lateral to medial over the iliopectineal eminence.
Snapping or clunking of the Iliopsoas can occur when the hip is brought from a flexed and abducted position (frog leg position) to extension and is usually asymptomatic. When the snapping is painful, Iliopsoas tendinitis is a cause of anterior hip pain.
Psoas tendinitis can occur
- Following an acute injury
- Sports related
- Associated with femoro acetabular impingement.
- After total hip replacement
- After hip arthroscopy
The diagnosis can be made with clinical examination, but it is important to exclude an intra-articular cause of the snapping. An MRI arthrogram can be performed with a local anaesthetic. A local anaesthetic injected in the joint should usually not affect the psoas symptoms. Ultrasound can be used to assess the tendon of the Iliopsoas and to inject a local anesthetic in the psoas bursa for diagnostic pain relief.
Ultrasound guided injections are more effective for psoas tendinitis following total hip replacement than with idiopathic tendinitis.
When the symptoms are resistant to physical therapy, a psoas tenotomy or lengthening can improve the pain symptoms. For the experienced hip arthroscopist this is a relatively easy procedure.
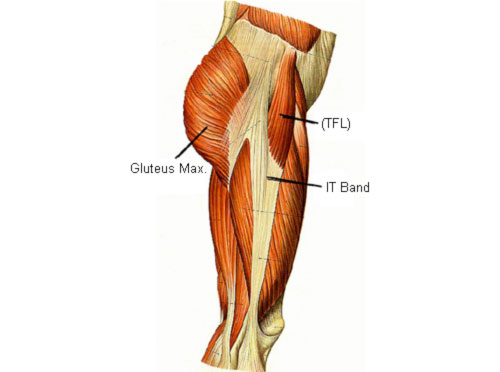
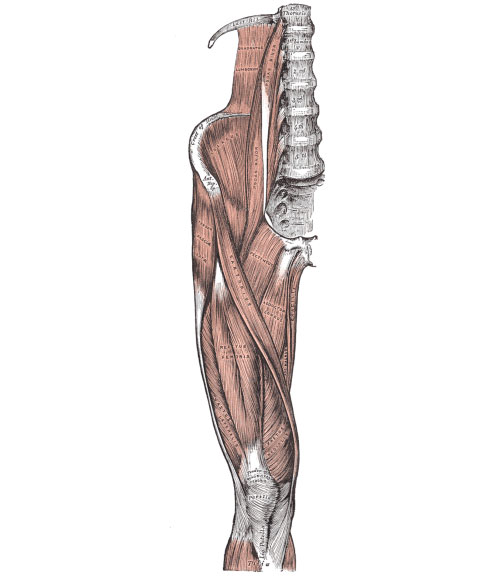
(Figure showing the muscles of the lateral side of the thigh.)
Snapping Iliotibial band
The Iliotibial tract is a fibrous band on the lateral side of the thigh, which runs from the iliac crest down to the knee. The ITB receives posteriorly a fibrous expansion of the Gluteus Maximus. The lateral type of snapping hip occurs when the Iliotibial band slides back and forward over the greater trochanter of the hip. This type is very common in adolescents and can be very painful and debilitating. When the ITB slides anterior of the greater trochanter, the patient can almost feel a spasm of his leg, which can only be relieved by traction on the leg and external rotation.
The diagnosis can easily be made clinically and by a dynamic ultrasound scan, which, in addition to the snapping of the hip, can also demonstrate inflammation of the underlying trochanteric bursa.
For quite a number of patients the symptoms can be so debilitating that they require surgery. Professor Schilders’ preferred technique is an endoscopic reconstruction of the ITB to stabilize the ITB and prevent further snapping.
Trochanteric Bursitis
Trochanteric bursitis is an inflammation of the trochanteric bursa. Wherever tendons run over bones, we find a bursa, a small jelly-like sac filled with some fluid between the bone and the tendon, which prevents damage to the tendon. The trochanteric bursa is interposed between the Iliotibial band and the greater trochanter of the hip.
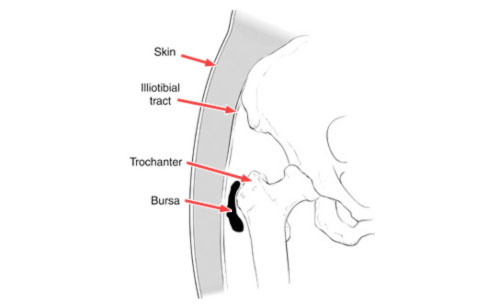
(Figure showing trochanteric bursitis (in black)
Trochanteric bursitis affects mainly middle aged or eldery people and is uncommon in young adults. Patients typically present with pain over the hip bone (trochanter). It is difficult to walk up and down slopes or raise up from a deep chair.
Patients experience pain at night and can’t sleep on the affected side.
The diagnose can easily be made clinically because of the location of the pain; an ultrasound scan or MRI scan can be used to assist with the diagnosis.
Conservative treatment usually provides pain relief and consists of intake of NSAIDs and modification of activities (avoiding activities that induce the pain). A steroid injection is very successful and can usually achieve an instant and permanent reduction of the symptoms. If the pain however returns, a repeated injection can provide further relief.
Surgical treatment is indicated for the patients whose bursitis is resistant to non surgical treatment, although it is important to exclude that the pain over the hip bone is not referred pain from the hip joint. Endoscopic treatment is now gaining more widespread acceptance and provides good outcomes.
Ligamentum teres tear
The ligament can tear with a hip dislocation, a fall on the lateral aspect of the hip or during a pivoting movement of the hip (similar to the mechanism of an ACL injury)
The torn ligament can get caught between the femoral head and the hip socket and can be responsible for pain and mechanical symptoms such as locking and catching. The ligament has been reported to heal spontaneously following a traumatic event, but this is unusual. There is no clinical test to diagnose this injury and therefore the diagnosis will depend on the suspicion of the experienced clinician.
The technique of choice to detect injuries of the ligament preoperatively is MRI arthrogram, although hip arthroscopy is the optimum method for the diagnosis.
Treatment currently consists of a hip arthroscopy and debridement of a partial or full thickness avulsion of the ligament. Although there are some early reports of reconstructions of the ligamentum teres, it can not be considered standard practice yet.